
March is Endometriosis Awareness Month
by Jennifer Pemberton
March is Endometriosis Awareness Month, and I want to take this opportunity to write about one of the most commonly undiagnosed and misdiagnosed illnesses associated with reproductive health.
It is estimated that 1 in 10 women of reproductive age, which is roughly 176 million women worldwide, have endometriosis. It is one of the leading causes of pelvic pain, infertility, and miscarriage. Yet, when I speak to others about endometriosis, many have never heard of it, or if they have heard of it, they associate the term with “bad cramps.”
What is endometriosis? Endometriosis gets its name from the endometrium, which is the tissue that lines the uterus that sheds during menses or becomes the placenta with pregnancy. When a woman has endometriosis, cells that resemble the endometrium exist outside of the uterus.
When these endometrium-like lesions exist outside of the uterus, they can cause irritation to the surrounding tissue, inflammation, and scarring. Endometriosis lesions are most common in the pelvis or on the outside of reproductive and other organs in the lower pelvis. Less commonly, endometriosis has been found in the diaphragm, and the lungs, among other places.
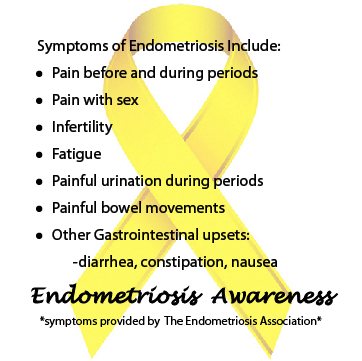
What are the symptoms of endometriosis? The most common symptom of endometriosis is pelvic pain, including increased pain just before and during menses. Some women experience pain throughout the menstrual cycle. Other symptoms include pain with urination or full bladder, bloating, nausea, constipation and/or diarrhea, pain with sex, infertility, and pregnancy loss. Although less common, some women experience few to no symptoms listed above.
How is endometriosis diagnosed? Endometriosis can be suspected from the report of symptoms. But, a definitive diagnosis can only be obtained through surgery and biopsy of suspicious tissue. Unfortunately, there is no blood test that can identify the presence of endometriosis lesions. Imaging tests rarely identify endometriosis, but it can be suspected from the distortion of anatomy caused by scar tissue or from the presence of endometriomas (also called a “chocolate cyst”) on one or both ovaries.
Why are there delays in diagnosis? The average time it takes from symptom onset to diagnosis has been reported from 6 to 12 years. When endometriosis goes undiagnosed and untreated, it can lead to more fibrotic disease, the worsening of symptoms, extensive adhesion-formation or scarring, and infertility. Why is there such a delay? It is probably a combination of factors including the lack of awareness about endometriosis, the stigma surrounding menses and women’s reproductive health, the dismissal of pelvic pain as “normal” pain associated with menses, pain language illiteracy, and the wide range of symptoms girls and women with endometriosis experience.
 What does endometriosis feel like? Most women experience discomfort just prior to and during menses that is best described as mild cramping. Over-the-counter (OTC) pain-relieving medications like Advil are generally sufficient to relieve normal menstrual cramping. Normal menstrual cramping rarely causes a girl or woman to miss out on important daily living activities, such as going to school or work, and lasts for a few days a month.
What does endometriosis feel like? Most women experience discomfort just prior to and during menses that is best described as mild cramping. Over-the-counter (OTC) pain-relieving medications like Advil are generally sufficient to relieve normal menstrual cramping. Normal menstrual cramping rarely causes a girl or woman to miss out on important daily living activities, such as going to school or work, and lasts for a few days a month.
Most women describe the pain associated with endometriosis as debilitating. It can include severe cramping just before and during menses. Some describe endometriosis pain as stabbing, burning, and/or like having hot nails dragged across the inside of the pelvis or barbed wire wrapped the midsection of the body. Some women experience minor symptoms at earlier ages, and their symptoms become more debilitating as they age and as the disease becomes more fibrotic and inflammatory. Some women have a sudden onset of severe symptoms. Because girls and women experience such a wide range of symptoms, this can also result in diagnostic delays.
What should you do if you suspect you have endometriosis?
1) Find a health care provider who listens to you and takes your pelvic pain seriously. Health care providers work for you. If they are not providing you with the services you deserve, seek other care.
2) Specifically, seek out an endometriosis specialist who has advanced laparoscopic excision surgical training.
3) Find a local and/or on-line support group. There are several groups on Facebook that provide support, information about surgeons and other health care providers, and up-to-date and accurate research on endometriosis and its treatment. Some are closed groups so your questions and comments will not be viewable on your public Facebook page. Here are a few I recommend: Specifically for girls, teens, and young women, ERC Girl Talk | Endometriosis Research Center | Nancy’s Nook | World Endometriosis Research Foundation | Endo Sisters Healing Together | Ask me About My Endo
4) Educate yourself about endometriosis. You must be your own health care advocate! Here are some sites I recommend to get started. Endometriosis.org | Endometriosis Research Center | The Center for Endometriosis Care | Center for Endometriosis Care News | Endopaedia | Endometriosis Foundation of America | World Endometriosis Research Foundation | Ask Me About My Endo
5) Surround yourself with family and friends who believe you and will help to support and nurture you through your treatment and ongoing health care. As much as possible, limit your interaction with those who are detrimental to your mental health and wellbeing.
6) Take care of your general health through good nutrition and regular exercise.
 Do birth control pills treat endometriosis? In short, no. While birth control can “mask” or lessen the symptoms of endometriosis, it does not treat or eradicate lesions from the body as antibiotics treat and eradicate infections. It is common for physicians to tell a young patient that some women just have more painful periods than other women and that this should not be concerning. Many times birth control pills do help. Physicians instruct the patient to take the birth control pills continuously and skip the “inactive” pills so that she does not menstruate. While the patient may report a reduction in symptoms from this course of action, birth control pills do nothing to treat her endometriosis. Some women do not get any relief from birth control pills.
Do birth control pills treat endometriosis? In short, no. While birth control can “mask” or lessen the symptoms of endometriosis, it does not treat or eradicate lesions from the body as antibiotics treat and eradicate infections. It is common for physicians to tell a young patient that some women just have more painful periods than other women and that this should not be concerning. Many times birth control pills do help. Physicians instruct the patient to take the birth control pills continuously and skip the “inactive” pills so that she does not menstruate. While the patient may report a reduction in symptoms from this course of action, birth control pills do nothing to treat her endometriosis. Some women do not get any relief from birth control pills.
Six months may pass, and a patient may return to her physician to say that her symptoms have returned. The physician may suspect endometriosis. The next course of action is to try a different kind of birth control pill. The physician may say or imply that maintaining her on birth control pills will prevent her suspected endometriosis from progressing. Unfortunately, this is not accurate. While birth control pills mask symptoms, the disease itself can progress, becoming deeper and more fibrotic.
 A patient may be maintained on birth control pills for years without ever having an official diagnosis other than “bad menstrual cramps.” And, it is only when the patient quits taking birth control that she comes to experience the full progression of the disease. It is at this point that physicians recommend an “exploratory” surgery to determine what is causing a patient’s symptoms. And, it is only at this time that she is diagnosed with endometriosis, often with extensive inflammation and scarring or adhesions. The doctor informs her that there is no cure and that her fertility may be compromised all to the dismay of the patient who believed her problem was that she was one of the unlucky women to have worse-than-typical “menstrual cramps.”
A patient may be maintained on birth control pills for years without ever having an official diagnosis other than “bad menstrual cramps.” And, it is only when the patient quits taking birth control that she comes to experience the full progression of the disease. It is at this point that physicians recommend an “exploratory” surgery to determine what is causing a patient’s symptoms. And, it is only at this time that she is diagnosed with endometriosis, often with extensive inflammation and scarring or adhesions. The doctor informs her that there is no cure and that her fertility may be compromised all to the dismay of the patient who believed her problem was that she was one of the unlucky women to have worse-than-typical “menstrual cramps.”
Does pregnancy cure endometriosis? No. Although some physicians still tell patients that pregnancy will make their symptoms better or cure their endometriosis, this is a myth.
What are other available treatments? After being diagnosed with endometriosis, a physician may offer further hormonal treatments, as it is commonly believed that there is no cure other than hysterectomy or menopause. Not wanting to undergo further surgery, a patient may take other hormonal medications. Like birth control pills, other hormonal medications such as these may mask symptoms for a period of time but often at the cost of significant side effects and financial strain. When the treatments are discontinued, a patient’s symptoms commonly return.
At the time of diagnosis during a laparoscopy (a surgery where small, “keyhole” incisions are made, one in the belly button through which a laparoscope–a thin, lighted magnifying scope a surgeon can use to visualize internal organs–is placed), an ob/gyn may attempt to treat the endometriosis surgically. These methods destroy the surface layer of the disease while leaving a large portion of the lesion untreated. When a woman’s symptoms do not improve, get worse, or return a few months after surgery, her physician often tells her that endometriosis always “grows back” and has no cure. Does a hysterectomy cure endometriosis? No. As endometriosis is by definition located outside the uterus, removing the uterus does not remove the disease.
What is the best course of treatment? Early diagnosis and excision surgery with a surgeon trained in the advanced laparoscopic excision of all endometriosis lesions. Unlike other treatments, excision involves using scissors or laser to dissect, remove, and send to pathology every suspected endometriosis lesion. When an entire lesion is removed down to its root, recurrence is less likely than with other methods that “burn the surface” of the lesions. Many women are restored to full health and have complete remission of their symptoms after conservative excision surgery that removes the endometriosis lesions, dissects adhesions, and corrects the anatomical distortion of reproductive organs caused by scar tissue while preserving the reproductive organs whenever possible. While excision surgery is the gold standard of current treatment options, when endometriosis is left untreated, it can create adhesions, muscle spasms, and other sequela. Some women will be left with scar tissue and pelvic floor dysfunction, which can continue to cause pain, especially pain with sex, and bowel and bladder dysfunction. A patient’s recovery can be aided with the help of a physical therapist who specializes in women’s health and with changes in diet and nutrition.
What can you do to spread awareness?
 1) Talk about endometriosis, reproductive health, and menstruation whenever there is an opportunity! Talking about menstruation helps to de-stigmatize and dispel myths about menstruation and pelvic pain.
1) Talk about endometriosis, reproductive health, and menstruation whenever there is an opportunity! Talking about menstruation helps to de-stigmatize and dispel myths about menstruation and pelvic pain.
2) March is endometriosis awareness month, and yellow is the color for endometriosis awareness. Wear yellow or a yellow ribbon during the month of March.
3) This year, many endometriosis sisters are also taking the Endo Challenge and turning their profile pictures on their Twitter and Facebook pages yellow during the month of March.
4) March in the Worldwide Endometriosis March taking place in many cities across the globe on March 28th.
5) Support efforts to include endometriosis as part of girls’ education about reproductive health.
6) If you are in college, bring educational resources from some of the sources I listed above to health care providers at your college and/or university or organize an educational talk about endometriosis on your campus. There are many in the endo community who are more than willing to participate in these efforts.
All too often health care providers and even family members and friends see women, especially young women, who complain of pelvic pain as attention- or drug-seeking whiners. When a woman’s pain is not taken seriously, not only can it negatively impact her health, it can also negatively impact her education, career, and relationships. As pelvic pain diminishes these other aspects of a woman’s life, increasingly health care providers, family members, and others come to interpret her failings as representative of psychological and emotional disturbance. Her reports of pelvic pain are interpreted as weakness and as secondary to and symptomatic of her primary psychological and emotional disturbance, all at a cost not only to the young woman’s life but also to our society as her disease remains undiagnosed and untreated.
We must work to spread awareness as much as possible. There is too much at stake. I have seen many girls and women driven to despair when chronic pain disrupts their lives. You never know. You may be saving a girl or woman’s life by talking about endometriosis!
2 thoughts on “March is Endometriosis Awareness Month by Jennifer Pemberton”